Key Takeaways
- Credentialing verifies healthcare providers’ qualifications and usually takes 60 to 180 days, depending on the provider and organization type.
- Initial credentialing takes about 3 to 6 months, while recredentialing happens every 2 to 3 years and is faster, typically 2 to 4 months.
- Factors like timely document submission, verification delays, staffing, and complexity of provider backgrounds affect how long credentialing takes.
- Starting early, staying organized, centralizing information, and using expert credentialing services can significantly speed up the process.
In healthcare, time is often the difference between serving patients and waiting on the sidelines. For doctors, nurses, and other providers, one important step before they can begin treating patients or billing insurance is credentialing.
Credentialing is the process that verifies a provider’s qualifications — including their education, training, licenses, work history, and any disciplinary records. It’s how hospitals, insurance companies, and regulatory bodies make sure providers meet all professional and legal standards.
While this process is essential for patient safety and trust, it can also take a lot longer than most expect. Delays in credentialing can mean weeks or even months before a provider can start practicing or get reimbursed for their services. That’s why understanding how long credentialing takes and the factors that affect it & why it is so important.
In this article, we’ll break down the typical timelines, what steps are involved, and how providers can speed up the process to get to work faster.
What Is Credentialing?
Credentialing is a formal process used by hospitals, clinics, and insurance plans to verify a healthcare provider’s qualifications—including education, training, licensure, work experience, malpractice history, and disciplinary actions.
These credentials are confirmed through primary source verification, meaning the organization contacts the original sources, such as medical schools, licensing boards, and the National Practitioner Data Bank (NPDB), to ensure accuracy and legitimacy.
This process ensures that providers meet professional standards and are qualified to safely treat patients. Staff like credentialing coordinators or specialists collect the provider’s documentation and prepare it for review by credentialing committees.
Typical Credentialing Timelines
The credentialing process can be time-consuming because it requires collecting and verifying various documents from education institutions, state licensing boards, and professional organizations.
Healthcare providers must complete different types of credentialing, such as initial credentialing and periodic recredentialing, to remain compliant and prove their ongoing qualifications.
On average, credentialing ranges from 60 to 180 days, depending on factors like the complexity of the provider’s credentials, the type of healthcare organization, and payer requirements.
Initial credentialing usually takes three to six months, including about two to four weeks for preparation, 60 to 120 days for application review, and another two to four weeks for final enrollment.
Recredentialing, which happens every two to three years, tends to be quicker, generally lasting two to four months. This consists of four to six weeks of preparation and 30 to 90 days for payer review.
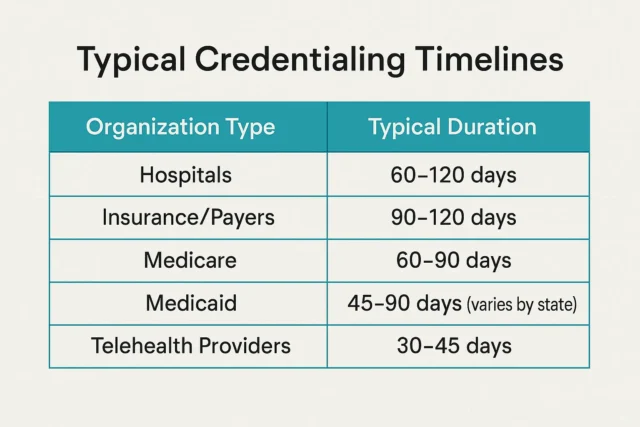
These timelines also vary by organization type: hospitals typically require 60 to 120 days, payers take 90 to 120 days, telehealth providers complete it faster in 30 to 45 days, Medicare falls between 60 and 90 days, and Medicaid usually takes 45 to 90 days.
What are the Factors Affecting Credentialing Duration?
Several things can make the credentialing process take longer or shorter:
How Fast Providers Submit Documents
If providers don’t send all the required papers or if the information has mistakes, it takes longer to fix and verify everything. Quick and accurate document submission helps speed up the process.
Waiting for Outside Verifications
Credentialing teams must verify information with schools, licensing boards, previous employers, and other groups. Sometimes these organizations take time to respond, which can delay credentialing.
Workload and Staffing
When there are many applications and not enough staff to handle them, credentialing may slow down. Manual processes without automation also take more time.
Complex Provider Backgrounds
Providers with licenses in multiple states, special certifications, or past malpractice issues require more checks, which can add extra time.
Type of Organization and Insurance Rules
Different places like hospitals, insurance companies, or telehealth services have their own rules and timelines. This affects how long credentialing takes.
State Rules and Busy Times
Some states have specific regulations, and busy seasons or insurance panel closures can cause delays.
How Can You Accelerate the Credentialing Process?
By following these steps, you can reduce delays and get yourself ready to see your patients sooner:
Start Early and Be Organized
Begin the credentialing process at least 4 to 6 months before the expected start date. Gather all necessary documents like licenses, education, work history, and malpractice records ahead of time. Being well-prepared helps avoid last-minute delays.
Here is a Sample Checklist for a New Healthcare Provider
- Complete the credentialing application form.
- Submit a government-issued photo ID, such as a driver’s license or passport.
- Provide your Social Security Number or Tax Identification Number.
- Submit your educational qualifications, including your medical school diploma, residency or fellowship certificates, and Continuing Medical Education (CME) certificates if applicable.
- Include all current licenses and certifications, such as your state medical license, DEA certificate, CPR/ACLS/BLS certification, and board certification if applicable.
- Provide a detailed work history for the past five to ten years, including explanations for any employment gaps.
- Include references from previous employers or supervisors.
- Disclose any disciplinary actions, sanctions, or legal issues.
- Submit supporting documents such as your National Provider Identifier (NPI) number, Medicare and Medicaid enrollment, and signed consent forms.
Centralize Provider Information
Keeping credentials stored securely in one place and using standardized digital profiles helps avoid repeating verifications. Centralized systems save time when providers need to credential with multiple organizations.
Hire an Expert Credentialing Services
Outsourcing credentialing to specialized teams with expertise and technology can significantly reduce turnaround times. Contacting these experts who know the common pitfalls and have established relationships with payers and credentialing bodies.
Conclusion
Credentialing is an essential step that ensures healthcare providers are qualified and ready to deliver safe patient care.
While the process can take anywhere from a few weeks to several months, understanding the typical timelines and factors that affect credentialing can help providers and organizations plan better.
Starting early, staying organized, centralizing information, and being proactive throughout the process are all important ways to avoid unnecessary delays. Because credentialing involves many detailed verification steps with multiple organizations, it can be complex and time-consuming.
To make this process faster and smoother, healthcare providers and organizations should consider hiring expert credentialing services.
These professionals have the experience, technology, and connections needed to handle credentialing efficiently, reducing wait times and allowing providers to start seeing patients sooner.
Choosing a trusted credentialing service is one of the best ways to speed up onboarding and focus more on delivering quality care.
FAQ
Insurance credentialing generally takes about 3 to 6 months (90 to 180 days). This time includes preparing documents, verifying credentials, committee approval, and final contracting. Some common estimates are around 90 to 180 days, but it can take longer depending on the provider and insurance company.
Credentialing takes time because verifying a provider’s qualifications involves checking many documents, like licenses, education, work history, and malpractice records with different organizations. Delays happen if documents are incomplete, if third-party verifications take long, staff are busy, or the provider’s background is complex. Committee meeting schedules and contract negotiations also add to the length.
Getting approved by Medicare usually takes between 60 and 90 days. This process includes submitting applications, verification, and review by Medicare officials.
Credentialing can be denied if there are issues such as incomplete or inaccurate information, disciplinary actions, malpractice history, expired licenses, or failure to meet the payer’s requirements. Sometimes background checks reveal problems, or the provider does not meet the standards set by the insurance company or health system.
Usually, it takes about 2 to 6 months (60 to 180 days), even if the provider is already licensed. The organization still needs to verify all credentials and work history, which takes time. If paperwork is complete and there are no issues, it may be done faster.
